Banner Section
Five Challenges to Successful Delivery of Health Care Projects
Points of View - Inner
Five Challenges to Successful Delivery of Health Care Projects

The current state of America’s health care system can be defined by one word: chaotic. New rules and regulations under the general umbrella of ‘health reform’ are overwhelming health plans and providers in the public and private sectors. In response, organizations are forging new partnerships, vendors are producing more and more ‘solutions’, and leaders are desperately building new strategic roadmaps even as the industry’s future, dramatically impacted by political agendas, is unclear. Simultaneously, we are fortunate to be part of the most dynamic and highly-impactful time in health care’s history.
Chaos creates significant challenges in organizations struggling to manage effective projects aimed at re-tooling, re-directing and re-building. The ability to successfully deliver strategic, operational and infrastructure-focused projects, necessary to support industry changes, is at risk. An equally impactful challenge organizations are facing is identifying those programs and projects that are strategic imperatives and should be prioritized as critical. Not addressing these core challenges can result in misalignment between delivery model and reimbursement, failure to meet key regulatory dates such as ICD-10, and the loss of good resources as they leave to join higher functioning organizations.
Through our consulting practice we have come to understand the challenges specific to the delivery of projects and have formulated broad guidelines to address effective project delivery in the health care industry.
Five Project Delivery Challenges
We have observed five significant challenges specific to health care project delivery. These challenges and their negative impact to project success are discussed below:
1. Ineffective / Non-Existent Portfolio & Project Management
With so many competing priorities in health care, organizations struggle to prioritize the most strategically and operationally impactful projects. Often, organizations lack an objective, consistent, criteria-based process to compare project opportunities and make decisions based on organizational constraints, strategic vision and regulatory imperatives. Furthermore, difficult trade-offs must be made between care delivery projects and those focused on administration or operations. As a result, important projects do not have adequate budget, suitable resources are scarce, and delivery is late and does not meet expectations.
2. Lack of Skilled Resources
As health care’s landscape changes, so do the type of resources required on successful projects. The current trend of adopting the Project Management Office (PMO) framework does not always equate to the ability to successfully lead multi-organization projects[1] , work side by side with clinicians to change care delivery (e.g., meaningful use) or assess the impact of a significant regulation (e.g., ICD-10). A project team without the necessary skills and experiences, including health care industry expertise, will ultimately fail.
3. Poor Vendor Management
Managing project vendors (e.g., software vendors, professional services vendors) effectively and efficiently is critical to project success and often overlooked. As new vendors flood the industry, promising the ‘right’ solution, organizations often fail to invest time to develop and manage the vendor relationship. Without strong upfront vendor relationships, critical issues may not be resolved efficiently, thus delaying the project and/or impacting the budget.
4. Limited Project Metrics & Data
While health care has traditionally been less data-rich and data-driven than other industries, there is a renewed (and legislated) emphasis on capturing a broad range of data to drive decisions, evaluate outcomes and trend improvements. Given the historic lack of data, organizations are challenged to develop metrics and use data to regularly measure the ‘health’ of a project. The impact is the inability to quantify risks to project success to immediately mitigate then proactively apply these learnings to future projects.
5. Deficient Change Methodology
The pressure to change rapidly is especially palpable in health care, as organizations that historically ‘grew into’ change now must employ change methodology to be successful. Often, projects do not include a work stream dedicated to preparing the organization for significant change. Change communication is particularly challenging due to the political dichotomy between physicians and administration / operations. The result is lack of understanding, acceptance and ultimately adoption of the change, leading to failed project outcomes.
Solutions
Our clients face some, if not all, of these challenges. We are frequently asked to turn-around failing projects, and have experienced these challenges first hand. Through our consulting practice and experiences, we have formulated broad guidelines to address effective project delivery in health care.
1. Successful project portfolio management requires all of the following:
- Empowered leadership who are also engaged participants.
- Organization-wide acceptance of the definition of ‘project’.
- Objective criteria in which to rank projects (including ROI).
- The capability to say ‘no’ or ‘later’ to project requests.
- Budget and resource constraint transparency.
Overall, the entire organization needs to accept and adopt the portfolio management process, so it is not bypassed and therefore rendered ineffectual.
2. Staff your project with the appropriate resources by following these steps:
- Identify the skills, experiences and time commitment required for your project.
- Perform a gap analysis between project needs and availability of resources with those skills.
- Close the gap by hiring temporary resources, provide training to build the skill sets in-house and/or bring in a professional services firm to do the work in partnership with your resources, training them throughout the project.
- Engage the Project Portfolio Management process if a resource gap still exists, to re-confirm project and resource priorities with other projects.
Balancing resource constraints (experience, skill set and availability) with project needs is most effectively driven by an organizational-wide, up-to-date resource-tracking matrix.
3. Manage project vendor relationships beginning from the inception of the contract, using the techniques below:
- Develop a solid working relationship with vendor leadership early on and maintain it; this relationship is vital when critical issues arise necessitating escalation.
- If the vendor delivery timeline slips, jointly develop an action plan with the vendor to get back on schedule, then manage them against the plan.
- Confirm vendor-supplied resources are committed for the duration of the project (as appropriate), to avoid vendor resource ‘drop and swap’.
- Request frequent status reporting, including transparency on internal vendor issues impacting project delivery scope and timeline, then jointly manage the risks.
4. Establish and measure project success criteria, following these recommendations:
- During the project planning phase, develop measureable and quantitative criteria to define project success. Include interim measurements to demonstrate the project is ‘healthy’ and moving in the right direction.
- Ensure that all team members and stakeholders understand and agree with the success criteria; this is a critical step that cannot be overlooked.
- Confirm that the data needed for measurement is available; if not, develop creative processes to obtain this data.
- Create and routinely publish the success criteria as a dashboard to executive stakeholders to serve as a reminder of how success is defined, to track project ‘health’ and confirm the criteria remains viable.
Refer to our Point of View: Warning Signs of Project Failure and Resolution Methods .
5. Apply rigorous change methodology to projects with significant impact to your organization, using these techniques:
- Engage change agents at all levels of your organization. Even when change is initiated ‘top down’, strategically placing advocates accelerates adoption and identifies pockets of resistance. Consider these resources members of your project team.
- Clearly and transparently describe the ‘future state’ and the organizational and individual benefits of achieving this state then, using various channels, communicate, communicate, communicate. When you are finished, communicate again.
- Throughout the project, as possible, generate ‘quick wins’ to demonstrate that positive change is proceeding. Actively solicit feedback on the change and incorporate the useful feedback into the project.
- Offer ample training on the future state, to build employee confidence, acceptance and adoption.
Refer to John P. Kotter’s seminal book on this topic, “Leading Change” for prescription, action-oriented change processes.
Framework for Success
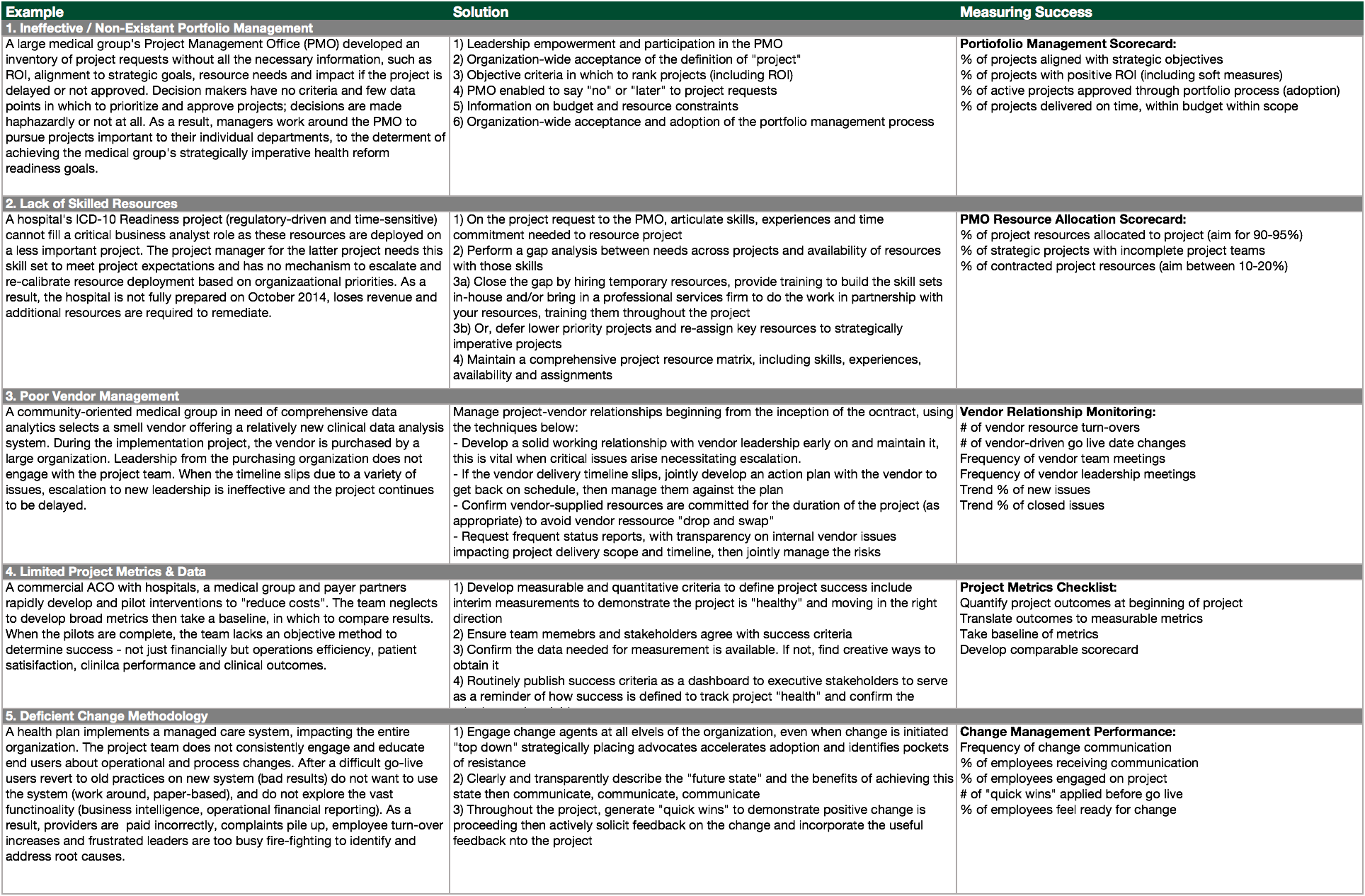
The following framework details real-life examples of each challenge, a prescriptive solution and specific measures to confirm a successful outcome:
Conclusion
We are engaged in a fascinating time in health care. Change is being driven at the federal, state and local level, in the public and private space, from foundations and private entities. Successful project delivery is at the heart of implementing change. Proactively addressing these five challenges using these techniques and guidelines will improve your project outcomes.
About the Author
Shani S. Trudgian is a Director at Kenny & Company and has over 20 years consulting experience with Accenture, Deloitte and Freed Associates. As a thought leader and industry advisor, Shani has guided her clients through health reform readiness strategy, ICD-10 readiness approach, ambulatory heath care delivery refinement, business model analysis, organizational development, change leadership and in other strategic areas.
Shani’s industry experience includes medical groups/IPA, hospitals, health plan (public/private), safety net clinics, department of public health, dental insurance, oral health delivery, non-profit grant-making philanthropy, and behavioral health organizations.
About Kenny & Company
Kenny & Company is a management consulting firm offering Strategy, Operations and Technology services to our clients.
We exist because we love to do the work. After management consulting for 20+ years at some of the largest consulting companies globally, our partners realized that when it comes to consulting, bigger doesn’t always mean better. Instead, we’ve created a place where our ideas and opinions are grounded in experience, analysis and facts, leading to real problem solving and real solutions – a truly collaborative experience with our clients making their business our business.
We focus on getting the work done and prefer to let our work speak for itself. When we do speak, we don’t talk about ourselves, but rather about what we do for our clients. We’re proud of the strong character our entire team brings, the high intensity in which we thrive, and above all, doing great work.
Notes
1. Accountable Care Organizations (ACO) frequently require multi-organization project teams
This article was first published on www.michaelskenny.com on May 23, 2013. The views and opinions expressed in this article are provided by Kenny & Company to provide general business information on a particular topic and do not constitute professional advice with respect to your business.
Five Challenges to Successful Delivery of Health Care Projects by Shani Trudgian, Kenny & Company is licensed under a Creative Commons Attribution-NoDerivs 3.0 United States License.







