Banner Section
Harnessing the Predictable in an Unpredictable Reality
Points of View - Inner

In the summer of 2013, the United States was preparing for the implementation of the largest health care reform package in more than 50 years, California announced details of the enrollment system that would be used to enroll upwards of 2.5 million newly eligible individuals into the Medi-Cal program or the newly established Covered California[1]. California was also taking on the massive task of transitioning hundreds of thousands of residents from the Low Income Health Program to the Medi-Cal managed care program[2]. With only months to go before the January 1, 2014 implementation date and changing enrollment system requirements, Medi-Cal managed care health plans and their delivery systems did not have time to fully prepare for the transition[3]. Despite the State’s genuine efforts to support Medi-Cal Managed Care Health Plans, the sheer size of the implementation, combined with the limited resources in state departments, led to preventable issues that impacted access to care and patient experience[4].
For health care organizations that insure, or provide health care to state or federally-run programs, the timeliness of clear business requirements associated with a major state-driven implementation such as Medi-Cal expansion is not always guaranteed, yet essential to provide high quality health care in a cost efficient way.
This phenomenon of challenging implementations caused by the lack of timeliness of business requirements is not limited to health care reform. Over the past decade, health plans have experienced numerous and significant changes to the public health coverage programs they offer. The transition of seniors, persons with disabilities to Medi-Cal managed care, the closure and transition of the Healthy Families Program[5] members to Medi-Cal, and the implementation of the Cal Medi-Connect[6] program are examples of some major implementations. Some local health coverage programs such as Healthy Kids Coverage Programs have either expanded, retracted, or closed[7].
Health care organizations that have a significant share of patients enrolled in publicly funded health coverage programs can adjust to the reality of ongoing, significant change with suboptimal time to implement. Health Plans and health care delivery organizations with a one or more publicly funded insurance products must respond quickly and efficiently to fickle payer requirements resulting from volatile public funding streams. We contend that organizations that develop rapid response teams, through playbooks developed from repeatable experiences, are better positioned to achieve high quality care and improved consumer experience, while reducing overall costs.
Publicly Sponsored Health Coverage Poses Unique Challenges
There is often a great amount of uncertainty in publicly sponsored health care resulting from the unpredictable forces of political differences, regulatory requirements, and perennial budget fluctuations. Additionally, health care in the U.S. and California in particular, is at an inflection point. Governments are reacting to the continuing increase in health care costs, more than a fifth of national government spending in 2015. Health care delivery systems are also reacting through a rapid growth in innovative ways to increase health care quality and improve patient experience while keeping costs under control. The uncertainty brought upon by the growth of innovation, without interventions to build upon what is certain, can lead to significant project management challenges causing employee dissatisfaction and impact member and provider experience.
Public health care-mandate implementations at the health care delivery level sometimes place member experience at a lower value compared to more pressing operational needs. For example, when organizations are faced with prioritizing two competing project tasks, the task of mass mailing notices to members to manage expectations will likely lose over integrating new claims procedures in a system of record. This consistent and sometimes necessary devaluing of member experience inadvertently leads to increased member grievances, lower member satisfaction, and in some instances, disrupts continuity of care.
For plans and provider networks, the uncertainty inherent in this environment trickles down to providers delivering health care to patients. Providers may inadvertently deny access to care due to delays in eligibility system file transactions and contract revisions. For example, pharmacies may deny critical access to medications resulting from delayed implementation of eligibility files transactions. All of which impact patients’ access to care.
The downstream effects of moving timelines, vague requirements, scope increases, and strict deadlines lead to a significantly greater risk of creating haphazard business processes. For example, in 2014, a few months prior to the requirement that Medi-Cal health plans were expected to provide non-specialty mental health services to their Medi-Cal members, some requirements necessary to establish processes between two or more agencies were still unclear. Despite this reality, health plans and the delivery system partners were charged with developing an infrastructure based on what was known at the time.
Despite these unique challenges, health plans and delivery systems that have a significant share of patients enrolled in publicly sponsored health coverage programs rely on standard project management approaches that may not be well suited for responding to this unique reality. The challenge is deepened further for some organizations who are at the early stages of adopting project management offices where project management resources are not yet viewed as a distinct function, and often competing with the actual delivery and business of health care.
The unpredictable nature of publicly sponsored health coverage programs should not prevent executives and directors from exploring innovative ways to manage these changes beyond industry standard tools. Instead, health care organization leaders can adapt their organization to fit this reality. In the next section, a framework will be introduced that organizations can adopt to manage efforts that improve member experience, employee satisfaction, and provider satisfaction.
Bringing Certainty to Uncertainty
What does our experience with publicly funded health coverage fickleness tell us? The most obvious is that requirements and mandates often present themselves with little notice and short timelines. Additionally, many of these requirements have similar and repeatable project tasks. Often organizations repeat these tasks but don’t archive project plans, build subject matter experts, sustain expectations among providers, and communicate to members using boiler plate approaches.
The approach being presented in this whitepaper shares many similarities with Agile[8] principles developed in the IT industry. Agile introduced a method in software development using both disciplined approaches and continuous refining, a departure from traditional project management. This was in response to software development in the 90’s always being late, over budget, and plagued by quality problems[9]; something becoming omnipresent in publicly funded health care.
To begin explaining the approach, we have identified levers commonly used by public entities to manage the implementation of health coverage mandates. Levers, in a mechanical sense of the word, is similar to an on or off switch where effort is placed on a switch to make the re-occurring and expected change happen. Levers in in our Rapid Response Team approach applies this concept to changes that often occur in publicly funded health care programs.
The following levers are not exclusive from one another and could occur simultaneously. The levers can be tailored to various environments and may consist of more or less than the four outlined below.
Member Growth or Loss: Adding or reducing a member/patient cohort to or from a health coverage program. May also include creating or closing a line of business. Examples:
- Medi-Cal Expansion as part of Health Care Reform.
- Mandatory Managed Care Medi-Cal for seniors & persons with disabilities.
- Healthy Families Program closure.
- Creation of Covered California as part of Health Care Reform.
- Reducing Healthy Kids[10] eligibility age limits.
Benefit Growth or Loss: Adding or eliminating a benefit for a health coverage program. Examples:
- Elimination of dental coverage for Adults on Medi-Cal.
- Addition of Adult Day Health Care centers benefits for Medi-Cal managed care.
- Addition of non-specialty mental health services to Medi-Cal managed care.
- Elimination of the Durable Medical Equipment (DME) benefit for a segment of Medi-Cal beneficiaries.
Member Transitions: When a cohort of individuals in one program is moved to another program; sometimes with a seamless transition expectation and with an objective of continuity of care. Examples:
- Healthy Families Program transition to the Medi-Cal managed care program.
- Transition of Medi-Cal seniors and persons with disabilities from fee for service Medi-Cal to managed care Medi-Cal.
- Transition of Low-Income Health Program participants into managed care Medi-Cal.
- Transition of dually enrolled Medi-Cal and Medicare members into Cal MediConnect.
Provider Payment Changes: Situations where payment amounts are reduced or increased. Also includes situations when payment schemes are modified. Examples:
- Ten percent rate reduction to Medi-Cal providers during State and Federal budget deficit years.
- Transition from ICD-9 to ICD-10.
- Rate increases for certain Medi-Cal member cohorts resulting from changes to benefits.
- Consolidation or re-organization of Medi-Cal payment rates (Rate Categories) and eligibility groups (Aid Codes).
- Conversion of fee-for-service to capitation payments models for a cohort of patients/members.
- Adding co-pays to the Medi-Cal program for children.
- Meaningful Use requirements.
The levers are developed through pooling the experiences of former project teams and subject matter experts involved with publicly funded coverage program changes. For organizations who possess little to no archival structure or a low level of institutional knowledge, a framework can be developed to begin collecting experiences with the intent to identify levers. Identification of these levers are an important step in the process towards developing playbooks and rapid response teams covered in the next section.
Project Playbooks and Rapid Response Teams
Playbook Development
Once levers have been identified, the rest of the playbook’s components and its respective tasks can now be developed. As noted in Figure 1, for each lever, repeatable components and their respective tasks used in past mandate implementations are identified. These tasks are developed and tailored based on an organization’s experience and unique structure. The tasks are then organized as components which are meant to reference a group of tasks associated with it.
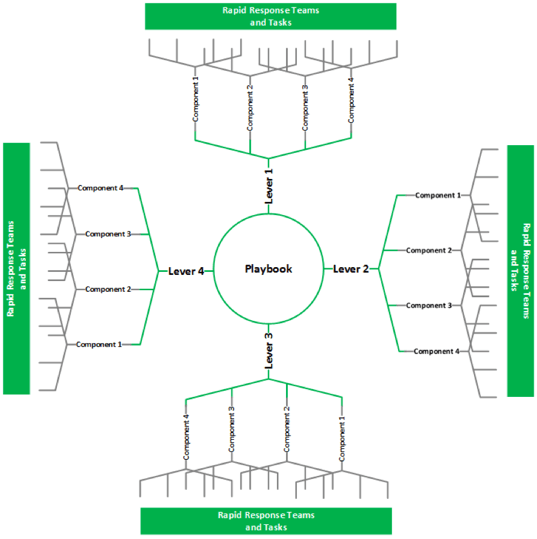
As shown in the Figure 1 Spider Diagram, playbooks are composed of levers, which are then composed of components. These components contain tasks which lead to the creation of Rapid Response Teams to execute them. In essence, components that are modular, repeatable and scalable in nature. The spider diagram also visually represents how order can be made from an unpredictable environment, very much like the publicly-funded health care landscape.
For example, if an organization’s line of business, such as Medi-Cal, is expected to grow its membership by 10% as a result of a new state law expanding program eligibility, most of the playbook tasks would fall under a few components.
- Provider Capacity: This includes the set of tasks involved with ensuring a delivery system and/or health plan has the current provider capacity to manage adding 10% more patients to provider panels without being out of compliance with state regulations. This could involve pursuing new providers to join the organization or identifying which provider panels have capacity and developing a mechanism to drive patients towards their direction. This may also involve provider communications tasks to manage expectations and to ensure general readiness among the provider community.
- Member Communications: This includes the mechanical tasks of budgeting, planning, and executing a mailing (or other forms of communications) to the target group of patients or members. This also includes the critical, but often overlooked, process of developing a message that maintains or improves member experience during the onboarding of new members or patients to your organization.
- Organization Capacity & Resourcing: A growth of 10% in patients or members could mean the need to hire more people to manage the increased volume. This component includes tasks to assess volume change impacts to the organization(s) and the proper response. It also includes skill gap analysis among existing employees if necessary. Tasks may also include training or provider seminars.
The step of identifying playbook components, made up of repeatable tasks, are then applied to all of the levers identified by an organization, as shown in Figure 2. This playbook can be in the form of documents or boiler plate Rapid Response Team plans and stored in a location, such as Microsoft Share Point, that is accessible to leaders throughout the organization. Playbooks should be revised as often as they are used by including a step in the project closure process to assess and revise playbooks.

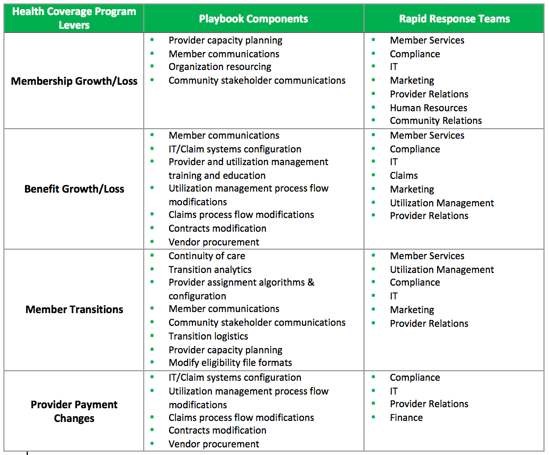
Figure 2: Playbook Components and Rapid Response Teams
Once a playbook is developed, an organization then determines which department or units are responsible for the components in a playbook’s levers. As shown in Figure 2 and using the same example of a 10% membership growth in Medi-Cal, units or divisions of an organization supply subject matter experts that would compose the Rapid Response Teams. These units have been identified using the same process of pooling the experiences of former project teams and subject matter experts to develop the health coverage program levers.
Rapid Response Team Utilization and Structure
Rapid Response Teams (RRT) are widely used in clinical settings to bring critical clinical care expertise to patients where ever it is needed[11]. The creation of these teams were developed in response to managing unstable patients and prevention of their unnecessary deaths. Research has supported RRT approaches in clinical environments with risk reduction rates as high as 80% for measures[12].

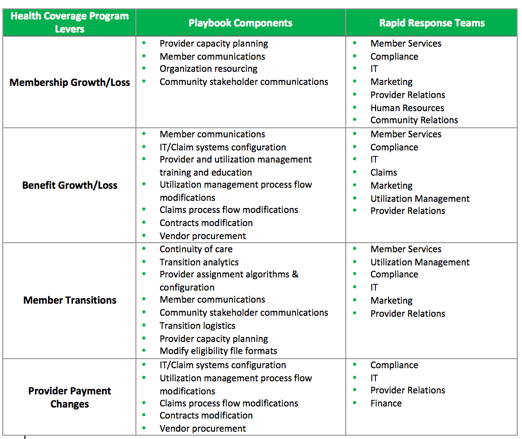
Figure 3: RRT versus Traditional Project Management in Changing Environments
While RRTs are often used in a clinical setting, our utilization of a RRT applies to project management approaches. As shown in Figure 3, RRTs differ from traditional projects in a few areas. First, traditional project management steps are significantly shortened and in some cases, completely bypassed. For example, the time used to build work breakdown structures at most would require refinement because the playbooks will have most, if not all, of the tasks necessary to execute components.
Secondly, the formation of teams in the RRT structure doesn’t occur in the same way as in the traditional project management approach. The RRT approach identifies team members in advance and only refines the composition when the project begins. For this reason, it is important for organizations that adopt RRTs to invest in their RRT members with the proper training, job responsibilities, and growth in subject matter expertise.
RRT members are not limited exclusively to managers, directors, or front-line staff. The components for a playbook often drives the skill requirements for the job at hand which may include front line staff in one component area to cover lower level tasks such as systems testing and a Director in another to cover high functioning tasks such as negotiating rates with providers.
Also, the RRT structure is led by a department where mandates are initiated and well understood. Because a large proportion of lever changes are mandates, Compliance and Regulatory departments are well-suited to be RRT leads. While it is intuitive to have Enterprise Project Management Offices manage all projects, RRT’s unique structure will thrive in a department that has subject matter expertise on requirements and the fluctuations that often occur during the implementation.
Lastly, the RRT utilizes project management tools to oversee the work. A traditional work plan with timelines, dependencies, and task owners are used, in addition to risk management tools. Success criteria are aligned to successful implementation of health care mandates defined by Compliance and Regulatory departments. The frequency and duration of meetings are similar to Agile Scrum models where there daily check-ins with RRT and weekly or biweekly meetings with RRT leads.
Rapid Response Team Advantage
With the increasing trend of value based reimbursement models coupled with the ongoing need to control health care costs, publicly funded sources are likely to continue at the pace we’ve experienced in the past decade. The California Department of Health Care Services (DHCS) and the Centers for Medicaid and Medicare Services (CMS) hint at, and in other cases, are very explicit of the changes coming to publicly funded health care in the coming years. For instance, the California HealthCare Foundation (CHCF) has taken the cue from these public agencies and health care industry trends and committed to focusing on consumer experience, value-based health care, and educating policy-makers[13]. Honing in on levers likely to present themselves in the near future is a strategy health care organization executives and leaders should consider to improve overall efficiency.
Putting the Rapid Response Team approach in action is where health care organizations will see benefits. As shown in Figure 4, the process of initiating a Rapid Response Team begins with an entity that has oversight for publicly funded health coverage programs, such as the Department of Health Care Services for Medi-Cal, and County Agencies which fund local based health insurance programs.
- Initiation: The State or Federal government makes a regulatory, compliance or funding change that impacts some aspect of a publicly funded health care.
- Identify Playbook Lever: Organizations then review requirements and determine if and which playbook lever(s) to utilize.
- Identify SMEs: The project lead or project sponsor then take the playbook lever and the pre-identified subject matter experts (SME) necessary to accomplish the playbook components. This step may also include adding SMEs to support new tasks not a part of the playbook but part of the requirements.
- Build RRT & Execute Project: Build the RRT and execute the project utilizing project management models suited for your organization.

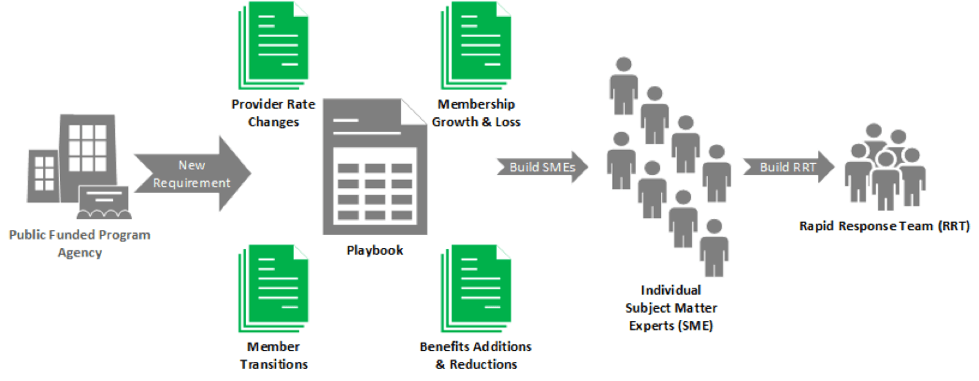
Figure 4: Activating the Rapid Response Team
When a Rapid Response Team (RRT) is activated, health plans and delivery systems see numerous benefits in employee satisfaction, member and provider experience. Additionally, RRTs cost less to implement compared to traditional project management and lead to increased accuracy during go-live.
The increased level of certainty brought about by playbooks and processes decreases the risk of employee dissatisfaction from reoccurring project management hardships. The lack of consistency, expectations, and static deadlines without a structure to properly manage a project results in employees sometimes taking the blame for external factors. Missing deadlines, compromising quality, and disorganization affects employee morale. When not addressed, these often lead to the expensive consequences of retaining high quality employees.
Member experience is also more likely to be addressed up front and compete less with operations that support health care delivery. Members benefit from a reduction in sub-standard internal operations resulting from haphazard process re-engineering in an environment where short timelines are omnipresent. Less grievances, improved brand, improved patient survey scores are just a few of the downstream benefits to a health care organization.
Among their main priorities, providers are more likely to be ensured they can continue to deliver care with minimal administrative interruptions from projects with many high risks, as often characterized by publicly funded health coverage programs. For instance, delays in developing or modifying electronic data interfaces to new requirements negatively impact continuity of care. Specifically, places of service such as pharmacies and primary care centers may deny health care services or medication if a system of record used to look up insurance status is not properly updated. Furthermore, mandates that have financial implications to providers are highly sensitive. A delay in claims process re-engineering or payment methodology changes will cause preventable delays in payments to providers.
Conclusion
There is often a great amount of uncertainty in publicly sponsored health care resulting from the unpredictable forces of political differences, regulatory requirements, and perennial budget fluctuations. This uncertainty, without interventions to build upon what is certain, can lead to significant project management challenges causing employee dissatisfaction, and impacts to member and provider experience.
Despite these unique challenges, health plans and delivery systems with a significant share of patients enrolled in publicly sponsored health coverage programs could adapt to this reality using the Rapid Response Team approach. The reality of the unpredictable nature of publicly sponsored health coverage programs should not prevent executives and directors from exploring innovative ways to manage these changes beyond industry standard tools.
Instead, health care organization leaders can adapt their organization to fit this unpredictable reality through harnessing what is predictable. By identifying health coverage program levers, developing playbooks, and incorporating the Rapid Response Team approach, health care organization can achieve high quality and improved health care experience, while reducing overall costs.
About the Author
Adrian Núñez is a Manager at Kenny & Company. He has over 13 years of leadership, operations, and management experience in publicly sponsored health coverage programs, managed care, and stakeholder management. He has participated in and guided organizations with program management, health care reform readiness and regulatory compliance, and enrollment & eligibility operations. He also has significant experience working with and development of community based networks, initiatives, advisory groups, and coalitions to achieve strategic goals. Adrian holds a Bachelor of Science in Biochemistry from University of California at Davis and is a graduate of the Coro Fellows Program in Public Affairs. Adrian can be reached at www.michaelskenny.com.
About Kenny & Company
Kenny & Company is a management consulting firm offering Strategy, Operations and Technology services to our clients.
We exist because we love to do the work. After management consulting for 20+ years at some of the largest consulting companies globally, our partners realized that when it comes to consulting, bigger doesn’t always mean better. Instead, we’ve created a place where our ideas and opinions are grounded in experience, analysis and facts, leading to real problem solving and real solutions – a truly collaborative experience with our clients making their business our business.
We focus on getting the work done and prefer to let our work speak for itself. When we do speak, we don’t talk about ourselves, but rather about what we do for our clients. We’re proud of the strong character our entire team brings, the high intensity in which we thrive, and above all, doing great work.
Notes
- Created as a result of health care reform in California, Covered California is a marketplace for people and small businesses to find out if they are eligible for financial help and buy health insurance, including Medi-Cal. www.coveredca.com
- Lytle EC, Roby DH, Lucia L, Jacobs K, Cabezas L, and Pourat N. Smooth Transitions into Medi-Cal: Ensuring Continuity of Coverage for Low Income Health Program Enrollees. Los Angeles, CA: UCLA Center for Health Policy Research, April 2013.
- “Mountainous Backlog Stalls Medi-Cal Expansion in California.” Helen Shen, July 2, 2014. Kaiser Health News.http://kaiserhealthnews.org/news/mountainous-backlog-stalls-medical-expansion-in-california.
- Health Consumer Alliance, comprised of more than 20 agencies sent a letter to Governor Jerry Brown. “Health Consumer Alliance’s Recommendations on Medi-Cal application backlog.” Letter signed on 2 July 2014.
- Healthy Families Program was a California and Federally funded health insurance program for children up to age 18. The program was eliminated due to budget constraints and children were transitioned into the Medi-Cal program.
- The state Medi-Cal program and the federal Medicare program partnered to create a three-year project to promote coordinated health care delivery to seniors and people with disabilities who are dually eligible for both of the public health insurance programs, or “dual eligible beneficiaries,” called Cal MediConnect. http://www.calduals.org/background/ca_duals_demo/
- Improving Coverage And Access For Immigrant Latino Children: The Los Angeles Healthy Kids Program Ian Hill, Lisa Dubay, Genevieve M. Kenney, Embry M. Howell, Brigette Courtot, and Louise Palmer Health Aff March 2008 27:550-559; doi:10.1377/hlthaff.27.2.550
- Agile is an umbrella term for iterative, incremental software development methodologies. See http://www.agilelearninglabs.com/ and http://en.wikipedia.org/wiki/Agile_software_development for further information.
- “The Best-Kept Management Secret On The Planet: Agile.” Steve Dunning. Accessed 16 April 2015. www.forbes.com.
- Healthy Kids programs are local health coverage programs funded by local funds to provide health insurance to children ineligible for state and federal programs.
- Establishing a Rapid Response Team. Institute for Healthcare Improvement. www.ihi.org. Accessed 20 March 2015.
- Bellomo R, Goldsmith D, Uchino S, et al. A prospective before-and-after trial of a medical emergency team. Medical Journal of Australia. 2003;179(6):283-287.
- “Taking Stock and Moving Forward.” Sandra R. Hernandez. California HealthCare Foundation. Accessed 13 April 2015. www.chcf.org/from-the-president/taking-stock-moving-forward.
This article was first published on www.michaelskenny.com on December 07, 2015. The views and opinions expressed in this article are provided by Kenny & Company to provide general business information on a particular topic and do not constitute professional advice with respect to your business.
Harnessing the Predictable in an Unpredictable Reality by Adrian Nunez, Kenny & Company is licensed under a Creative Commons Attribution-NoDerivs 3.0 United States License.







